Coronis Health, Emergency Medical Services
Emergency Medical Services Billing
At Coronis Health, we use the latest electronic medical billing techniques to ensure the highest returns for Emergency Medical Services possible.
From customized monthly reports to certified coding services, we have the top-notch experience and technology to optimize EMS billing collections for providers, including fire EMS, private ambulance facilities, volunteer squads, and hospital-based ambulance systems.
Hear What Our Clients Have to Say
Specialized Solutions, Global Capabilities
Free Billing & Collections Audit
We Find Missing Revenue In 95% Of Our Reviews.
Are you leaving money on the table?
– A comprehensive review of your complete revenue cycle
– Compare key metrics against industry benchmarks in your specialty and region
– Review A/R levels of care, CPT and insurance company plus aged receivables
Rate is based on collections volume

Case Studies
Emergency Medical Services Billing
Specializing in...
Testimonials
-
$20000000000
In Charges
-
$4700000000
In Payments
Size Matters! More is Always More!
Services

What Makes Us Different
At Coronis Health, we use the latest electronic medical billing techniques to ensure the highest returns for Emergency Medical Services possible. We go after the last dollar so you can focus on patient care. We are software agnostic, so our expert billers can start work on your system immediately. We specialize in getting claims out correctly the first time to avoid unnecessary claims.
Who We Serve
Coronis Health is proud to serve a variety of Emergency Medical Services (EMS) clients.
-
Hospital-Based Ambulance Systems
Coronis Health billing and collection practices boost collection rates and speed payments to hospitals. We’re ahead of the curve when changes and updates to federal or commercial insurance forms or policies are released, and we scrupulously maintain compliance with all HIPAA regulations, Red Flag rules, and all other federal, state, and local regulations that can affect your hospital-based ambulance service. Our up-to-date knowledge of regulations minimizes denials and ups your revenue.
-
Private Ambulance Providers
The Coronis team tailors claim management processes to meet clients’ specific needs, whether you treat 100 patients or 100,000 a year. We link concern and compassion for patients to your financial goals and regulatory requirements and target those issues that are specific to your privately run ambulance service. We offer global capabilities and high-touch service you won’t find anywhere else.
-
Volunteer Squads
New funding made available through cost recovery will be used to offset the rising costs associated with supporting your rescue squad and helping you to continue to provide the best possible services to the county and/or township citizens.
-
Municipal 911 Systems
At Coronis Health, your reimbursement does not begin with the submission of a claim. It begins with a defined and customized revenue recovery plan tailored to your municipal 911 system. We have a consistent track record of increasing your cash flow once your unique requirements and demands are identified through our free financial checkup.
-
Non-Emergency Providers
We consistently increase our clients’ efficiency via improved claims processing models, accounts receivable timelines, and decreased claims rejections. We are experts in benchmarking your specific needs, knowing how to increase your revenue cycle, and bringing you the peace of mind you rely upon to provide excellent service to your patients. Let us manage your medical billing so you can focus on what you do best: patient care.
-
Fire EMS
Coronis Health is a highly trusted and respected ambulance billing provider servicing a wide array of customers. We use the latest technology and a proactive and innovative billing approach proven to maximize revenue. This enables you to generate the earnings you need to acquire the necessary equipment and staff to serve the unique needs of your community and remain independent.
More About Coronis Health
What Emergency Medical Billing & Coding Services Do We Provide?
With more than 100 years of combined experience in the medical billing service industry, we’re able to offer our clients unmatched emergency billing services, such as:
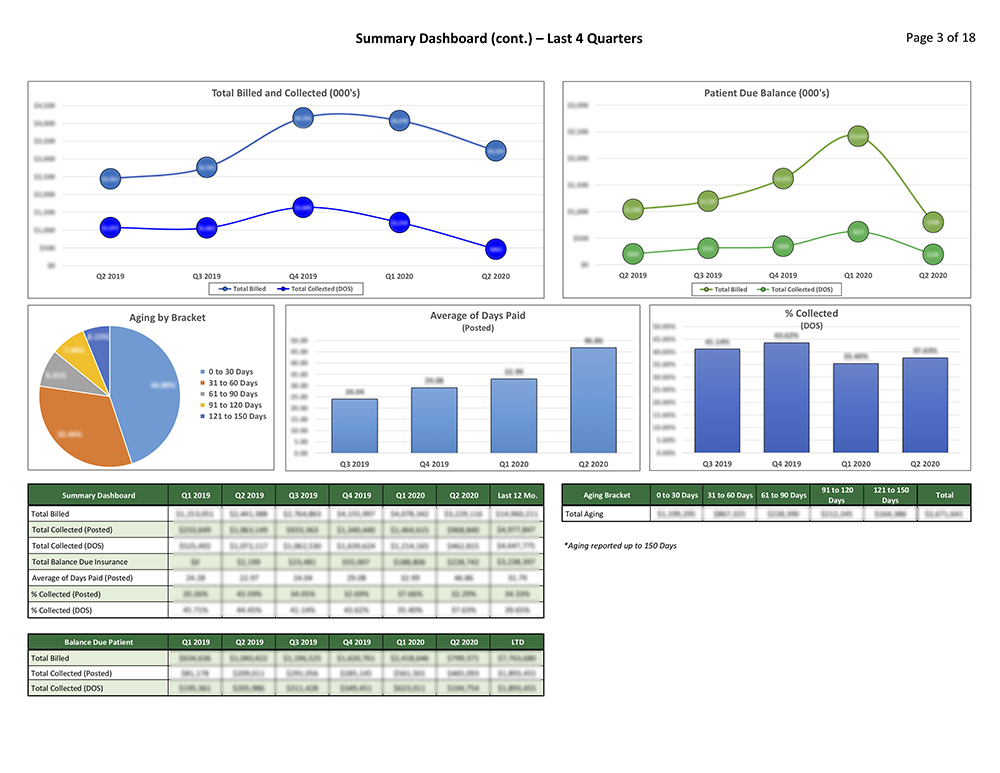
- Department Budgeting
- EMS Department Performance Statistics
- Managed Care Marketplace Evaluation
- Field Data Capture and Analysis
- Revenue Forecasting
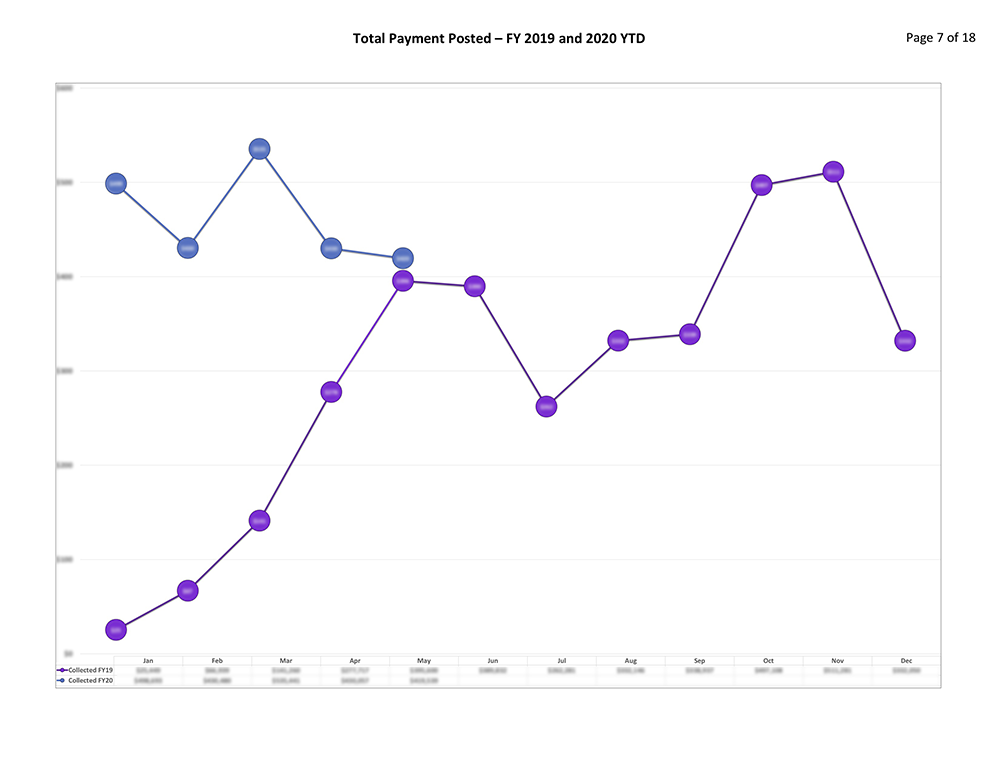
- Claims Status and Denial Management
- Claims Aging Reports
- Labor Resources
- Marketplace Penetration
- RAC Audit Liabilities Assessment
- Charge and Pricing Management
- Underpayment Analysis
- Payer Reimbursement Trends
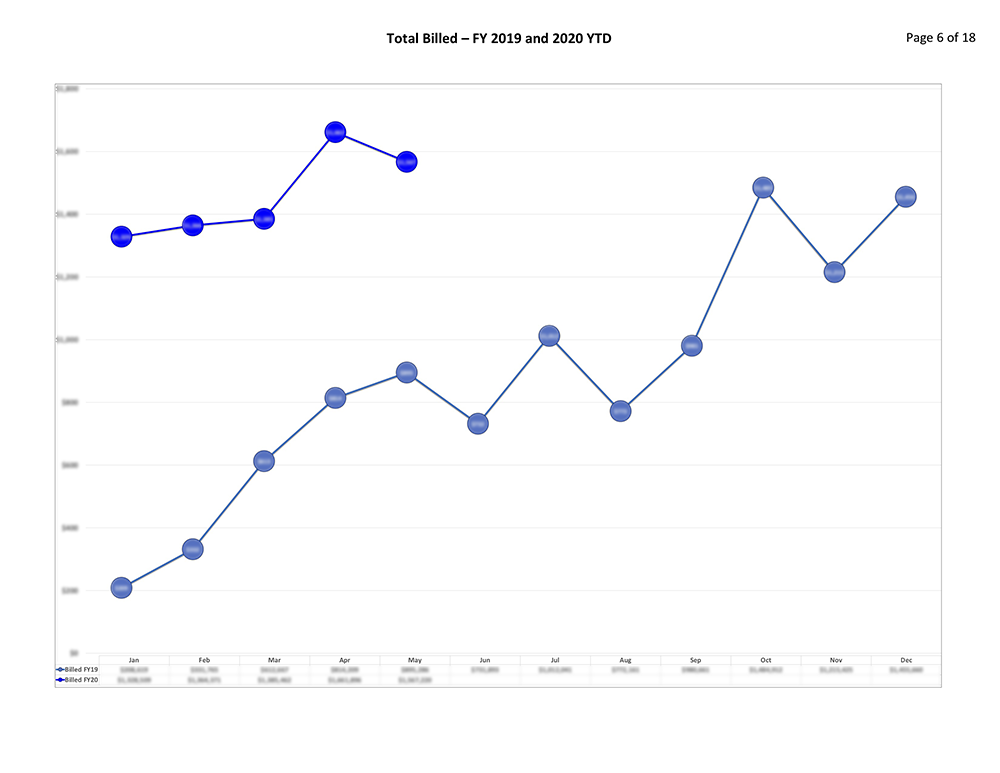
- Monthly Volume Reports
What You Need to Know about EMS Billing with Coronis:

-
Typical Issues Faced With ED Billing
Each medical speciality has its own unique billing challenges that can impact revenue, and emergency medical services are no different. One of the most complex issues in EMS billing stems from ED services, such as supplies, medications, reserved room time, and support staff. When emergency physicians code and bill separately from ED services, hospitals can inadvertently under report the actual services they provided to patients. These coding and billing mistakes aren’t just time-consuming to correct, they’re also likely to result in lost revenue.
-
Benefits of Using Coronis Health for Emergency Billing & Coding
Coronis Health has a proven combination of professional people, technology and detailed EMS industry experience. We speak EMS and our leadership has been in your shoes so we understand what is needed to perform at the highest level. Coronis Health truly becomes part of your EMS department and a trusted partner. We will provide meaningful and dependable solutions through time-proven billing and collections methods to increase your revenue while handling your claims in a timely and compliant manner.
-
What Your Emergency Services Consultation Will Look Like
Your emergency services consultation focuses on assessing your facility’s financial health and wellbeing. During your financial health checkup, we’ll perform a comprehensive analysis of your revenue cycle to identify deficiencies and make the appropriate modifications promptly. This data allows us to compare your metrics against industry standards and competitors in your field. With a comprehensive consultation, Coronis Health can also evaluate patient and insurance A/R charges, fee schedules, and more.
Contact Us To Outsource Your EMS Billing
Coronis Health has the best talent, technology, and resources to increase your total revenue. Contact us today to schedule a free financial health checkup to find out how our medical billing service can eliminate your claim denials and maximize your profits.