The fact is that anesthesia is no longer a free service to hospitals and ASC administrators. Most American anesthesia practices must receive substantial financial support to remain viable. It is the payment of hospital subsidies that changes the dynamic of the relationship; every transaction must reflect fair market value.
Since the highest cost of providing anesthesia service is the cost of its anesthesiologists, certified registered nurse anesthetists (CRNAs) and anesthesiologist assistants (AAs), having the ability to monitor and track provider productivity and operating room utilization are essential to effective management of the team. Developing the tools to capture and report productivity metrics consistently is a significant challenge that requires assiduous focus and commitment, which very few practices have truly mastered. There are two ways to report such data: (a) cases, units and hours of anesthesia care can simply be tallied by provider and by month (or any specified period of time), or (b) these measures can be normalized by day worked. The example below demonstrates the distinction. Normalized data is preferred for purposes of comparison and benchmarking.

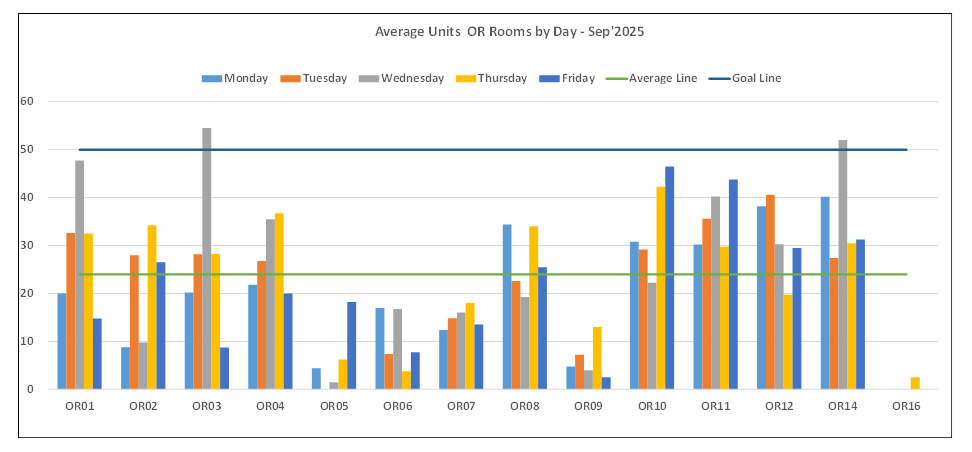
Normalized metrics reflect the average value per clinical day. In this example, if the target is 50 ASA units per day, then it is easy to identify that the room is underutilized. Typically, such calculations will only include weekdays, prime-time data and exclude after-hours and holidays. Usually, obstetric activity is not included in such calculations; however, this same methodology can be carried out for the step-down rooms to help determine efficiency levels later in the day. It should be noted that, even with optimal efficiency, support in the current market is necessary due to compensation levels. Furthermore, payer mix associated with billed units also plays a vital role in the potential shortfall of staffing any OR.
This same concept can be applied by anesthetizing location to identify which locations are consistently productive and which are loss leaders. Such information can be especially relevant to discussions with administration. Please see table below.
The ability to track activity by anesthetizing location can be especially useful but it requires some careful planning and quality control. The list of designated anesthetizing locations must be clearly defined and communicated with the billing staff. Each anesthesia record should identify where the case was performed. When such tracking is first implemented, it is typically necessary to implement a scorecard so that management can monitor the consistency and accuracy of provider documentation of anesthetizing locations. Fluctuations in where cases are performed throughout the day, as well as non-OR cases, can add a level of complexity in achieving reliable data capture that can help quantify performance in these areas. Special attention should also be paid to “specialty rooms” (i.e., cardiac and pediatrics) as these providers’ compensation includes an inflator over and above market, which drives up the cost of staffing the room even further.
The value of such management tools lies in their application. They are especially useful as a springboard for discussion of coverage requirements with administration, especially when the objective is efficient OR utilization. Operating room efficiency is the key to helping the facility manage costs amidst provider shortages. These shortages will not be relieved any time soon, so both the providers and the administration must adapt to the new norm.
