Per the HHS, A covered health care provider that wants to use audio or video communication technology to provide telehealth to patients during the COVID-19 nationwide public health emergency can use any non-public facing remote communication product that is available to communicate with patients. OCR is exercising its enforcement discretion to not impose penalties for noncompliance with the HIPAA Rules in connection with the good faith provision of telehealth using such non-public facing audio or video communication products during the COVID-19 nationwide public health emergency. This exercise of discretion applies to telehealth provided for any reason, regardless of whether the telehealth service is related to the diagnosis and treatment of health conditions related to COVID-19.
Under this Notice, covered health care providers may use popular applications that allow for video chats, including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, or Skype, to provide telehealth without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA Rules related to the good faith provision of telehealth during the COVID-19 nationwide public health emergency. Providers are encouraged to notify patients that these third-party applications potentially introduce privacy risks, and providers should enable all available encryption and privacy modes when using such applications.
Originating Site - An originating site is the location of an eligible Medicare beneficiary at the time the service furnished via a telecommunications system occurs. Beneficiaries are eligible for telehealth services only if they are presented from an originating site located in:
- A rural Health Professional Shortage Area (HPSA) either outside of a Metropolitan Statistical Area (MSA) or in a rural census tract or:
- A county outside of MSA
**COVID-19 UPDATE: EXPANSION OF TELEHEALTH WITH 1135 WAIVER: Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence starting March 6, 2020. A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, will be able to offer telehealth to their patients. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
Prior to this waiver Medicare could only pay for telehealth on a limited basis: when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the service.
Authorized Originating Sites – Effective 3/6/20 for 1135 Waiver:
- The offices of any physicians or practitioners
- Any Hospital
- Critical Access Hospitalists (CAHs)
- Rural Health Clinics
- Federally Qualified Health Centers
- Hospital-based or CAH-based Renal Dialysis Centers (including satellites)
- Any Skilled Nursing Facilities (SNFs)
- Community Mental Health Centers (CMHCs)
- Patient Home
Distant Site Practitioners – Practitioners at the distant site who may furnish and receive payment for covered telehealth services are:
- Physicians
- Nurse Practitioners (NPs)
- Physician Assistants (PAs)
- Nurse-midwives
- Clinical nurse specialists (CNSs)
- Certified registered nurse anesthetists
- Registered dietitian and nutrition specialists
- Clinical psychologists (CPs) and Clinical Social Workers (CSWs). CPs and CSWs cannot bill for psychiatric diagnostic interview examinations with medical services or medical evaluation and management services under Medicare.
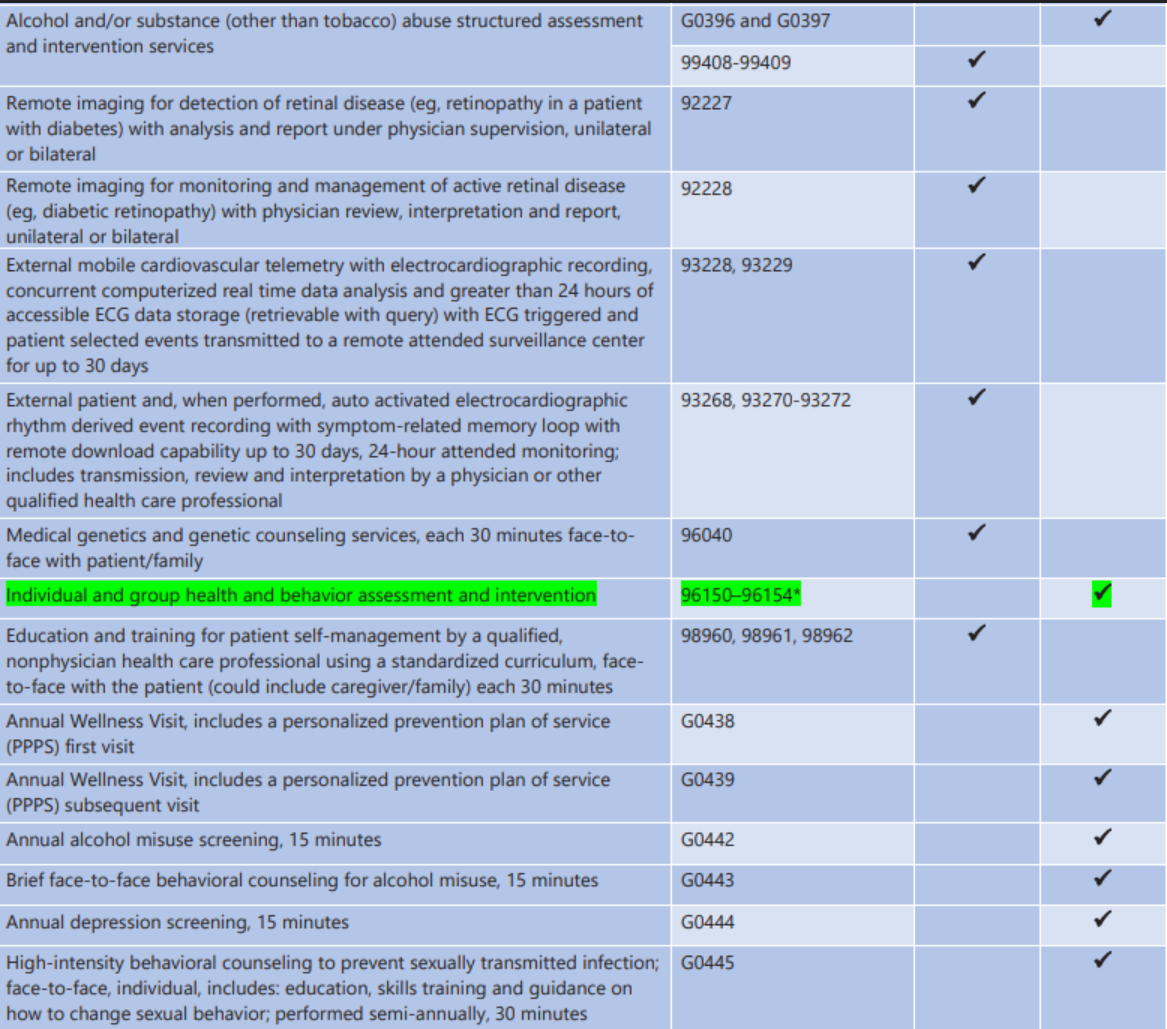
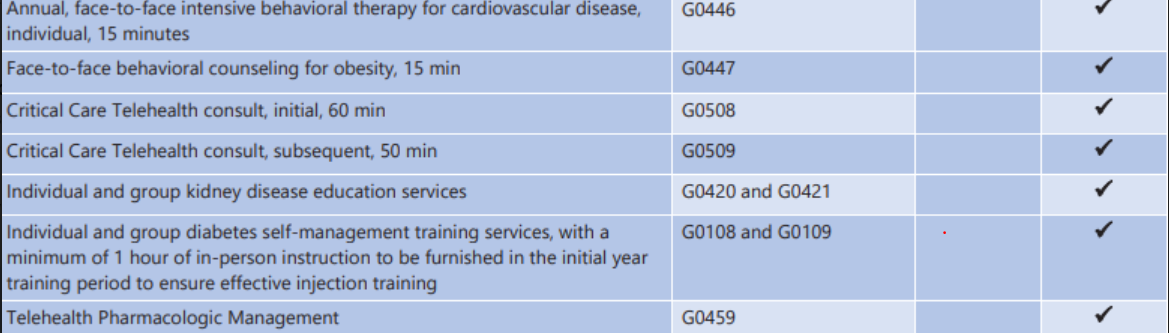
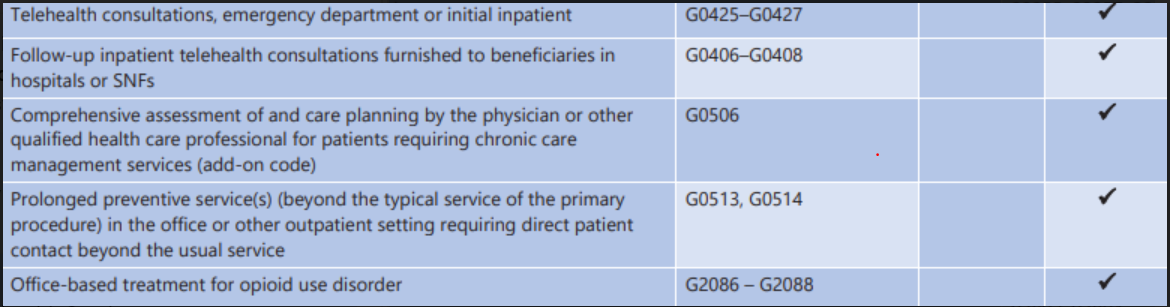
The reporting of telemedicine services varies by payer and state regulations. The below Table outlines the different coding and billing requirements whether you are the “hosting facility” or the “performing provider.”
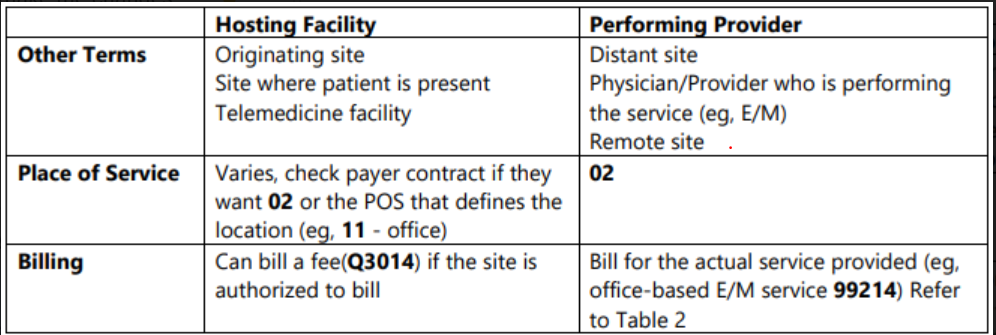
Hosting Facility- CMS requires reported telemedicine services to include both an originating site and a distant site. The originating site is the location of the patient at the time the service is being furnished. The distant site is the site where the physician or other licensed practitioner delivering the service is located. A telemedicine facility fee is paid to the originating site. Claims for the facility fee should be submitted using HCPCS code Q3014: "Telemedicine originating site facility fee." Originating sites include: the office of a physician or practitioner, Hospitals, Critical Access Hospitals (CAH), Rural Health Clinics (RHC), Federally Qualified Health Centers (FQHC), Hospital-based or CAH-based Renal Dialysis Centers (including satellites), Skilled Nursing Facilities (SNF), and Community Mental Health Centers.
Performing Provider Claims for professional services should be submitted using the appropriate service code (please table see below) and the modifier “95” or “GQ.”
Modifier - 95 modifier: Synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system. Append this modifier to an appropriate CPT code. GQ modifier: Providers participating in the federal telemedicine demonstration programs in Alaska or Hawaii must submit the appropriate CPT or HCPCS code for the professional service along with the modifier GQ, “via asynchronous telecommunications system.”
*NOTE: Medicare stopped the use of modifier GT in 2017 when the place of service code 02 (telehealth) was introduced. If payers reject a telehealth claim and the 95 modifier is not appropriate, ask about modifier GT.
Place of Service- For professional services furnished on or after January 1, 2018, to indicate that the billed service was furnished as a telehealth service from a distant site, submit claims for telehealth services using Place of Service (POS) 02: Telehealth: The location where health services and health related services are provided or received, through telehealth telecommunication technology.
*NOTE: It is important to be aware that CMS requires that the POS for the hosting facility align with the type of facility the site is. For example, if an outpatient hospital facility, use POS 22, if a private office, use POS 11.
Reimbursement - Medicare will reimburse the health professional delivering the telemedicine service will be reimbursed at the current fee schedule rate for the comparable in-person medical service
Medicare Virtual Check In Services - In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. We expect that these virtual services will be initiated by the patient; however, practitioners may need to educate beneficiaries on the availability of the service prior to patient initiation.
Medicare pays for these “virtual check-ins” (or Brief communication technology-based service) for patients to communicate with their doctors and avoid unnecessary trips to the doctor’s office. These virtual check-ins are for patients with an established (or existing) relationship with a physician or certain practitioners where the communication is not related to a medical visit within the previous 7 days and does not lead to a medical visit within the next 24 hours (or soonest appointment available). The patient must verbally consent to receive virtual check-in services. The Medicare coinsurance and deductible would generally apply to these services.
Doctors and certain practitioners may bill for these virtual check in services furnished through several communication technology modalities, such as telephone (HCPCS code G2012). The practitioner may respond to the patient’s concern by telephone, audio/video, secure text messaging, email, or use of a patient portal. Standard Part B cost sharing applies to both. In addition, separate from these virtual check-in services, captured video or images can be sent to a physician (HCPCS code G2010).
Medicare E-Visits Services - In all types of locations including the patient’s home, and in all areas (not just rural), established Medicare patients may have non-face-to-face patient-initiated communications with their doctors without going to the doctor’s office by using online patient portals. These services can only be reported when the billing practice has an established relationship with the patient. For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. The patient must verbally consent to receive virtual check-in services. The Medicare coinsurance and deductible would apply to these services.
Medicare Part B also pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. Practitioners who may independently bill Medicare for evaluation and management visits (for instance, physicians and nurse practitioners) can bill the following codes:
- 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes
- 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11– 20 minutes
- 99423: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes.
Technology – As a condition of payment from Medicare, you must use an interactive audio and video telecommunications system that permits real-time communication between you, at the distant site, and the beneficiary, at the originating site. In almost all cases, Medicare only reimburses for live telemedicine – in other words, a real-time video chat between a physician and patient. The idea is to model a face-to-face visit as closely as possible. Medicare also reimburses for store-and-forward telemedicine services, but only in Hawaii and Alaska.
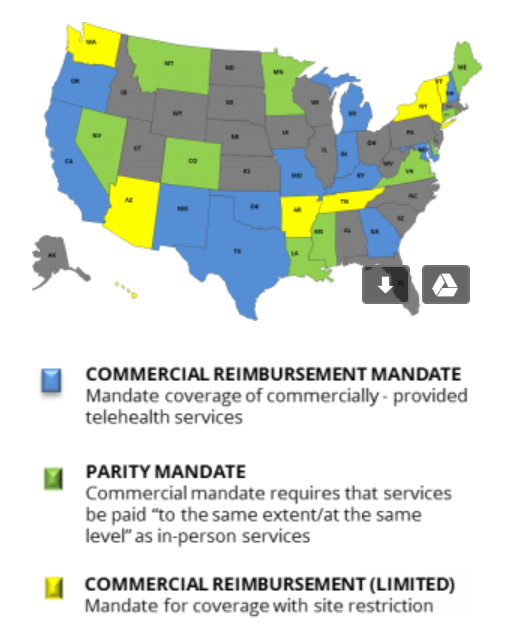
Medicaid – All 50 state Medicaid programs, have some type of telemedicine coverage. However, Medicaid differs from Medicare in that its policies vary from state to state; each state has flexibility to determine how it will reimburse for telehealth. The following website link displays Telemedicine coverage and reimbursement guidelines per state: https://www.americantelemed.org/initiatives/2019-state-of-the-states-report-coverage-and-reimbursement/
Commercial Payers – Private insurers – have been most aggressive in reimbursing for telehealth visits. Many national plans embrace this healthcare innovation and have been steadily broadening coverage through partnerships with telemedicine services companies.
Today, many states have parity laws (see map below) that mandate commercial payers provide comparable coverage and reimbursement for telemedicine services as in-person services.
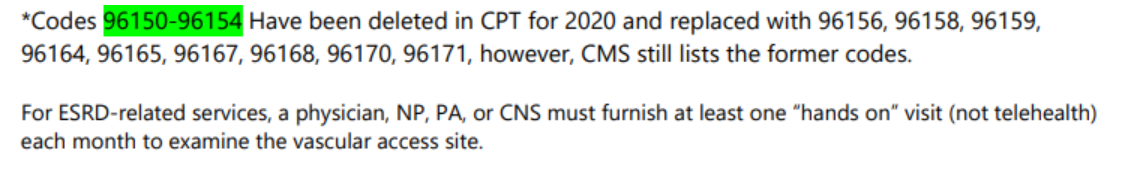
2020 Telehealth Services HCPCS/CPT Codes