Every year, approximately 15 million colonoscopies are performed in the United States. Few surgical procedures have experienced such anesthesia consideration and policy review. It has been an extensive evolution since the 1960s, the result of which has created one of the most profitable lines of business for anesthesia practices.
First, there was the refinement of the endoscope, which allowed for its universal adoption by endoscopists as the most effective tool to scan the colon and rectum and remove potentially cancerous polyps. Because of the nature of the procedure, anesthesia providers began to promote the ability to enhance the surgical experience with the use of propofol resulting in a more comfortable and clinically effective screening. As the volume of anesthetic cases rapidly expanded, the real question was whether anesthesia was really necessary. It took a Medicare policy update to confirm the value of anesthesia services and with this the flood gates sprang open: anesthesia providers flocked to endoscopy clinics like lemmings to the race.
As is so often the case, however, more volume meant more challenges, especially from payers who questioned the value of an additional charge for such a common procedure. The result has been new procedure codes and policy changes intended to manage the potential cost of the additional service. As the debate and policy revisions continue to unfold, colonoscopy revenue has become one of the most closely monitored aspects of anesthesia care.
THE EVOLUTION OF THE FLEXIBLE COLONOSCOPE
The procedure has a decades-old history with significant successive endoscopic innovations that eventually led to the development of the current colonoscope. Colonoscopy first commenced in 1960s, stemming from innovations in upper endoscopy. Gradual innovations into imaging technology, guideline developments and increased awareness led to increases in access and utility expansion. The first scopes were stiff and awkward to manipulate through the colon, but the current technology allows a complete screening of the rectum and colon, despite its curves and anatomical idiosyncrasies.
It is an optimal procedure for identifying precancerous polyps and recommended for screening individuals with risk factors, such as a family history of polyps or cancer. The impact of the current screening protocol greatly reduces the risk of colon cancer.
According to the American Cancer Society, the estimated incidence of colon cancer in the United States in 2023 is:
- 153,020 new cases
- 106,970: in the colon
- 46,050: in the rectum
Colorectal cancer is the second most common cancer diagnosed in both men and women in the United States. The incidence rates vary by age, race and ethnicity. For example, the rate is higher in older adults and among non-Hispanic white, African American and American Indian/Alaska Native populations.
The general lifetime risk of developing colorectal cancer in the United States is about 5% to 6%, with estimates around one in 23 men and one in 25 women, according to the American Cancer history, certain genetic mutations, inflammatory bowel diseases and specific racial and ethnic groups, can increase an individual’s risk above this general population average.
THE ROLE OF ANESTHESIA
While many endoscopists would provide their patients a degree of sedation, this was not always adequate and often impacted the quality of the screening. Anesthesia providers saw this as a great opportunity. Numerous clinical mishaps, such as the death of Joan Rivers, underscored the need for a separate provider to monitor the patient through the procedure.
Anesthesia is valuable in colonoscopy because it increases patient comfort and procedural safety, improves adenoma detection rates (ADR) and completeness of the procedure, and allows for better patient cooperation. While some procedures can be performed without it, anesthesia’s benefits in reducing patient discomfort and improving the quality of the examination often outweigh the associated costs, though there is ongoing discussion about standardization and appropriate use.
Key Benefits of Anesthesia in Colonoscopy
Patient Comfort and Safety:
- Anesthesia ensures patients are relaxed, comfortable and have little to no memory of the procedure, enhancing the overall experience. The anesthesia team monitors vital signs to ensure patient safety.
Improved Quality of the Procedure:
- Sedation provides optimal conditions for the endoscopist, which can lead to increased ADR and a higher likelihood of complete examination, including reaching the cecum and ileum.
Enhanced Patient Cooperation:
- Patients under anesthesia are less likely to move or be distressed, allowing for a more thorough and efficient procedure.
Facilitates Treatment:
- With a more comfortable and cooperative patient, procedures like polyp removal become more manageable and less likely to be perceived as painful by the patient.
- Most endoscopists will also admit that having a separate anesthesia provider allows them to be more efficient.
ANESTHESIA PAYMENT POLICY
As anesthesia providers started to get more involved with endoscopic procedures, the question of the day became simply will there be payment for anesthesia? Payer policies varied, and a number of major health plans refused to pay for anesthesia for endoscopic procedures. This became a source of considerable frustration. Then, in 2015, Medicare provided a definite answer with a policy announcement.
If you provide anesthesia for a Medicare patient undergoing a screening colonoscopy, you will be able to collect 100 percent of the allowable amount from Medicare and will not need to bill the patient for any co-payment or deductible, beginning on January 1, 2015. You must, however, identify the service as screening rather than diagnostic or therapeutic through the use of the appropriate modifier on your claim.
In the interest of making preventive care more widely available, a provision of the Affordable Care Act, Section 4104, waived “colorectal cancer screening test” co-payments and deductibles for Medicare beneficiaries. For the same reason—to avoid patient cost-sharing’s becoming “a significant barrier to these essential preventive services”—CMS extended the waiver of coinsurance and deductible to anesthesia services furnished in conjunction with a screening colonoscopy in the Final Rule on the Physician Fee Schedule for 2015.
This had a profound impact on the market. Acting on the assumption that, as goes Medicare, so go the rest of the payers, anesthesia providers began increasing their role in providing care for endoscopic procedures. All across the country, endoscopy became the new frontier.
NEW ENDOSCOPIC CODES
The Relative Value Guide (RVG), published by the American Society of Anesthesiologists (ASA), had included two ASA codes for endoscopic procedures: ASA 740 for upper GI procedures and ASA 810 for lower GI. Both had a base value of 5. In 2018, the CPT coding manual introduced five new codes for endoscopic procedures to replace the two historical codes. See Table 1.
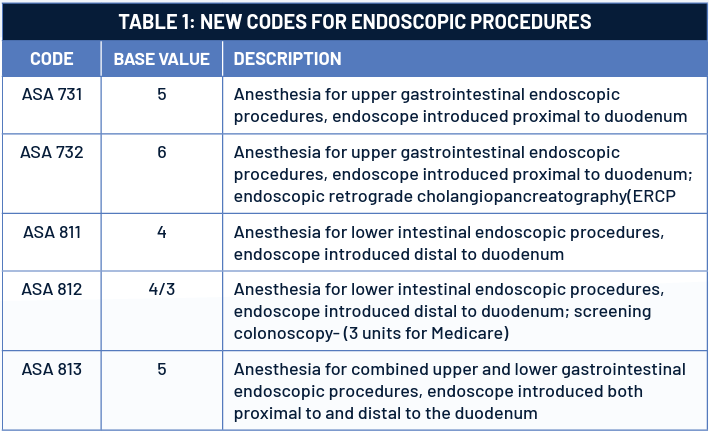
The focus of these new codes was essentially to lower the base value for lower GI procedures, including colonoscopy. The impact of these new codes resulted in about 10% reduction in endoscopic revenue. The curious issue here is that Medicare dropped the base value for 00812 to 3 units. As is so often the case, new codes are designed to help control and manage the revenue potential of these procedures.
THE NET IMPACT OF POLICY CHANGES
A review of five years of data for colonoscopies from ten large Coronis Health clients indicates the basic trends of this part of the business. The majority of patients have commercial insurance, which pays well. Medicare patients represent about one-third of all cases at discounted Medicare rates. Self-pay patients with no insurance are a very small piece of the overall pie. See Table 2.
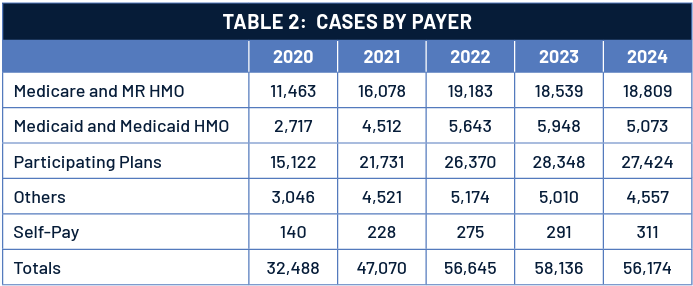
The volume of colonoscopies started to grow in 2020, just before the pandemic. But once it ramped up, case volumes have been quite consistent.
As is often the case, Medicare and Medicaid rates have a significant impact on the overall net yield per case. Payer mix is always determinative in the calculation of the profitability of the service. As indicated in Table 3, the overall average yield per case is approximately $260. Clearly, the efficiency of the venue and the average number of cases performed per day is the most critical factor in determining profitability.
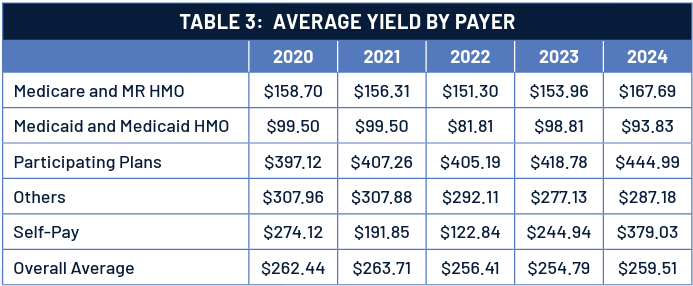
This review clearly demonstrates the potential value of endoscopy to the anesthesia practice. The thing to remember is that success in endoscopy is all about volume and efficiency of the clinic.
FINAL THOUGHTS
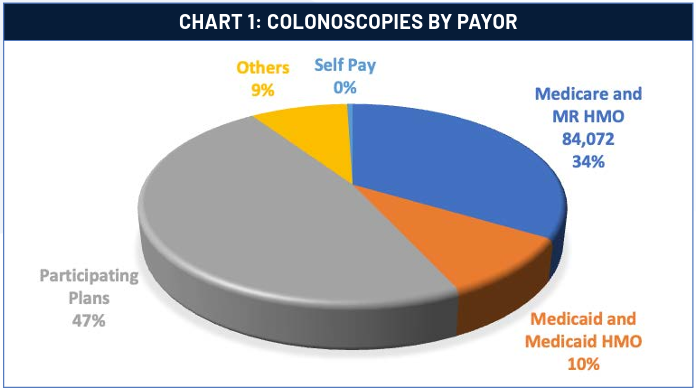
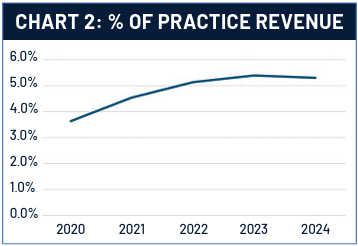
As Chart 2 indicates, about 5% of most practice revenue comes from colonoscopy, and this trend is gradually increasing. In other words, endoscopy is always likely to be an important component of an anesthesia practice, despite inevitable payer policy changes.
The evolution of anesthesia payment for endoscopy is a typical case study but is not unique. Managing an anesthesia practice optimally is a never-ending process that requires constant vigilance and attention to detail
Jody Locke, MA serves as Vice President of Anesthesia and Pain Management Services for Coronis Health. Mr. Locke is responsible for the scope and focus of services provided to Coronis Health’s largest clients. He is also responsible for oversight and management of the company’s pain management billing team. He is a key executive contact for groups that enter into contracts with Coronis Health. Mr. Locke can be reached at jody.locke@coronishealth.com.
