Conversion Factor
To recap what we previously published, there will be two RBRVS (non-anesthesia) conversion factor rates for 2026: one is for providers participating in an alternative payment model (APM), such as an accountable care organization, and the other is for those who do not participate in an APM. For most physicians—meaning, those who do not participate in an APM—the non-anesthesia conversion factor is $33.4009, which reflects an increase of 3.26% over against the current (2025) RBRVS conversion factor.
Telehealth
Below is a summary of what the final rule provides in terms of telehealth services, beginning in 2026:
- Medicare rejected the request to add the AMA’s newly adopted telehealth codes (98000-98015) to Medicare’s approved list of telehealth codes. In other words, Medicare will not reimburse the AMA’s telehealth codes.
- The telehealth flexibilities allowed during COVID-19 are not extended by the final rule. Congress extended some of these only until January 30 (in most cases) of next year. After that, without further legislative action, the flexibilities are ended. This means that, beginning January 31 of 2026, Medicare will require the patient to be at a medical facility or in rural areas to receive such services.
- Medicare is making permanent the ability of teaching physicians to have a virtual presence in all evaluation and management (E/M) visits where there is a 3-way visit with the (a) teaching physician, (b) resident, and (c) patient in 3 different locations. Furthermore, the documentation must indicate the parts of the visit the teaching physician attended, which must include the portions of the visit that determine the billing level, i.e., medical decision-making or time.
- The final rule allows virtual direct supervision—where the billing physician or practitioner (e.g., PA, NP) is immediately available via an interactive, two-way audio-video communication device (excluding audio-only)—for incident-to services, except those with a 10-day or 90-day global period. The virtual availability of the supervising clinician should be documented in the medical record in such cases.
- Medicare clarified that remote physiologic monitoring (RPM) and remote therapeutic monitoring (RTM) are not telehealth services as they are inherently non-face-to-face. This means that a telehealth place-of-service code would not be used for RPM and RTM services.
- The final rule permanently removes frequency limitations to subsequent inpatient visits, subsequent nursing facility visits, and critical care consultations done via telehealth.
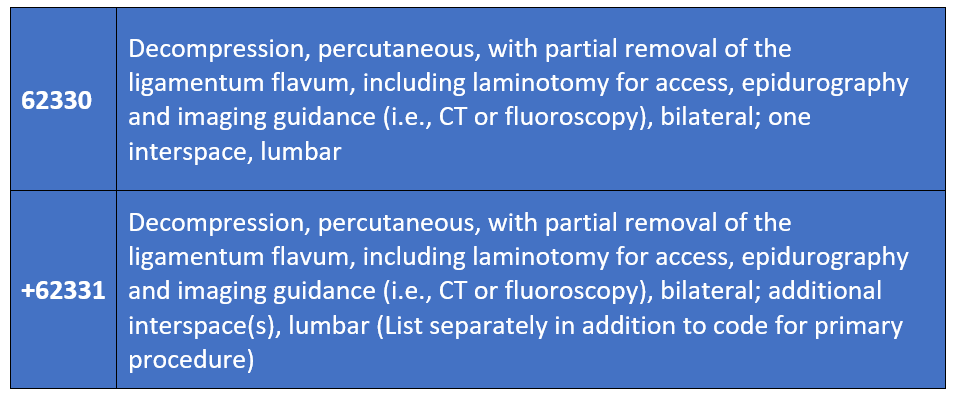
New Codes
Chronic pain practitioners will have two new codes available in 2026. These will replace the deleted code 0275T for the MILD procedure. Below are the new codes, along with their descriptors.