Conversion Factor
As required by statute, 2026 marks the first year where the calculating of the RBRVS (non-anesthesia) conversion factor and the anesthesia conversion factor will be based on whether or not the provider was a qualifying participant (QP) in an alternative payment model (APM). So, in other words, beginning next year, there are to be two different conversion factors for RBRVS and two different conversion factors for anesthesia. Since the vast majority of our readers are not QPs in an APM, we will only be listing herein the conversion factors for RBRVS and anesthesia that reflect the non-QP numbers.
The proposed 2026 RBRVS (non-anesthesia) conversion factor is $33.42. This represents a projected increase of $1.07, or 3.32%, from the current conversion factor of $32.35. This would apply to all non-anesthesia services, such as acute pain blocks and invasive line placements. In part, the above increase is based on a temporary 2.5% increase in physician payments for 2026, as authorized in the recent budget reconciliation package passed by Congress. Our readers may recall that physician payments were reduced by 2.83% in 2025 after a temporary increase in payments for 2024 expired.
The proposed 2026 anesthesia conversion factor is $20.57. This reflects a 1.3% increase from the current anesthesia conversion factor of $20.31. While modest, this does represent a long-awaited increase for the anesthesia community who had heretofore been suffering from years of proposed decreases in the conversion factor. Nevertheless, the American Society of Anesthesiologist (ASA) remains unimpressed with this progress, writing in a recent publication:
ASA is disappointed with these woefully low payment updates included in the CY 2026 PFS proposed rule. These updates will not provide much relief for the physician practices that are struggling to cover their costs. The proposed rule underscores how the Medicare payment system is broken, especially during a time when anesthesia groups are faced with continued inflation pressures. ASA will continue to engage legislative stakeholders and regulatory agencies to erase this negative impact on anesthesiologists.
Yes, things can always be better; but at least the government is not proposing another decrease in reimbursement.
Efficiency Adjustment
The proposed rule calls for the application of an efficiency adjustment to the work RVU and corresponding intra-service portion of physician time of non-time-based services that CMS expects to accrue gains in efficiency over time. CMS is proposing to use a sum of the past five years of the Medicare Economic Index (MEI) productivity adjustment percentage to calculate this efficiency adjustment, which would result in a proposed efficiency adjustment of -2.5% for 2026.
Practice Impact
Despite the positive updates to the conversion factors, CMS estimates that anesthesia, when the effect of all policies are taken into account, will be negatively affected at the rate of 1.0%. This is based on Table 92 of the proposed rule, where the rule’s impact on the various specialties is estimated. These impacts ranged from -6% for Infectious Disease to +7% for Allergy/Immunology. While anesthesia took a small hit, chronic pain gained a respectable 3.0% positive impact, from a reimbursement perspective.
Curiously, the Table makes it clear that these specialty impact estimates do not take into account the changes in the conversion factors.
Telehealth Services
For 2026, CMS is proposing to streamline the process for adding services to the Medicare Telehealth Services List. The agency plans to simplify the review process by removing the distinction between provisional and permanent services and limiting the review on whether the service can be furnished using an interactive, two-way audio-video telecommunications system. Here are the specific proposals for 2026:
- Permanently remove frequency limitations for subsequent inpatient visits, subsequent nursing facility visits, and critical care consultations.
- For services that are required to be performed under the direct supervision of a physician or other supervising practitioner, permanently adopt a definition of direct supervision that allows the physician or supervising practitioner to provide such supervision through real-time audio and visual interactive telecommunications (excluding audio-only).
- Except for services that have a global surgery indicator of 010 or 090, a physician or other supervising practitioner may provide such virtual direct supervision for applicable incident-to services under § 410.26, diagnostic tests under § 410.32, pulmonary rehabilitation services under § 410.47, cardiac rehabilitation and intensive cardiac rehabilitation services under § 410.49.
- End the current policy allowing teaching physicians to have a virtual presence for purposes of billing for services furnished involving residents. Rather, the proposed rule looks to transition back to the pre-PHE (public health emergency) policy, which required that, for services provided within metropolitan statistical areas (MSAs), teaching physicians must maintain physical presence during critical portions of resident-furnished services to qualify for Medicare payment. (The rule would maintain the rural exception established in the CY 2021 PFS final rule.)
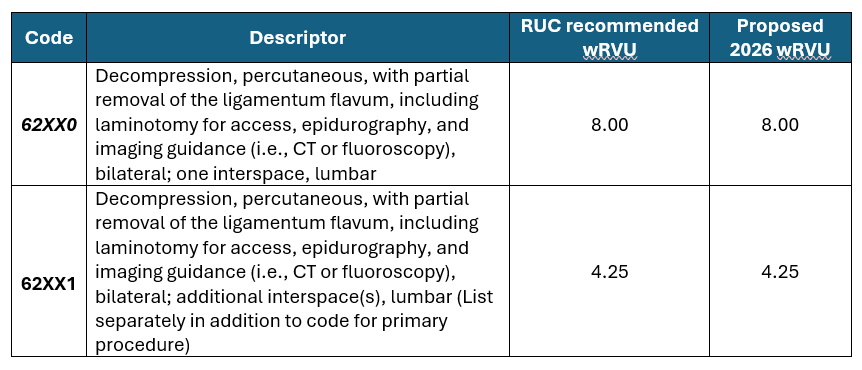
New Chronic Pain Codes
According to the ASA, starting January 1, 2026, pain medicine physicians will be able to get paid by Medicare for Lumbar Decompression services using the new category I PILD CPT codes (62XX0 and 62XX1). For 2026, CMS has proposed the following work RVUs for the PILD codes, which are the same as the RUC recommended value. The table provided by the ASA below reflects CMS’s proposed work RVUs for these new service codes. Code 0275T will be deleted.
We will have additional updates from the proposed rule in coming weeks, including what CMS may have in store for its quality programs.
