Evaluation and Management
The 2025 PFS final rule now also allows payment of the office/outpatient (O/O) evaluation and management (E/M) visit complexity add-on code, Healthcare Common Procedure Coding System (HCPCS) code G2211 when the O/O E/M base code (99202-99205, 99211-99215) is reported by the same practitioner on the same day as an annual wellness visit (AWV), vaccine administration or any Medicare Part B preventive service, including the Initial Preventive Physical Examination (IPPE), furnished in the office or outpatient setting.
Telehealth Services
Absent Congressional action, beginning January 1, 2025, the statutory limitations that were in place for Medicare telehealth services prior to the COVID-19 public health emergency (PHE) will “retake effect for most telehealth services,” according to the final rule fact sheet published by the Centers for Medicare and Medicaid Services (CMS). These include geographic and location restrictions on where the services are provided, and limitations on the scope of practitioners who can provide Medicare telehealth services.
Based on information provided by a CMS representative, no telehealth service can be billed where the patient is in their own home unless the service involves one of the following: mental health disorder, substance abuse disorder, or ESRD assessment. That means for telehealth services other than these three exceptions, the patient will need to be in an “originating site,” which essentially means a physician’s office or facility in a rural area. In those limited circumstances where a telehealth visit may be billed for a patient in their home, the final rule still allows an interactive telecommunications system to include two-way, real-time, audio-only communication technology for any Medicare telehealth service furnished to a beneficiary in their home, if the distant site physician or practitioner is technically capable of using an interactive telecommunications system, but the patient is not capable of, or does not consent to, the use of video technology.
CMS will continue through 2025 to permit distant site practitioners to use their currently enrolled practice locations instead of their home addresses when providing telehealth services from their home.
The final rule adds several services to the Medicare Telehealth Services List, including caregiver training services on a provisional basis and PrEP counseling and safety planning interventions on a permanent basis. CMS will continue the suspension of frequency limitations for subsequent inpatient visits and critical care consultations for 2025.
The rule permanently adopts, for certain services, a definition of direct supervision that allows the supervising physician or practitioner to provide such supervision via a virtual presence through real-time audio and visual interactive telecommunications.
- The supervising physician or practitioner may provide such virtual direct supervision (a) for services furnished incident to a physician or other practitioner’s professional service, when provided by auxiliary personnel employed by the billing physician or supervising practitioner and working under his or her direct supervision (and for which the underlying HCPCS code has been assigned a PC/TC indicator of “5” and services described by CPT code 99211), and (b) for office or other outpatient visits for the evaluation and management of an established patient who may not require the presence of a physician or other qualified healthcare professional.
- For all other services furnished incident to that require the direct supervision of the physician or other supervising practitioner, the rule allows direct supervision to be provided through real-time audio and visual interactive telecommunications technology only through December 31, 2025.
Teaching physicians will continue to be allowed to have a virtual presence for purposes of billing for services furnished involving residents in all teaching settings, but only in clinical instances when the service is furnished virtually (for example, a three-way telehealth visit, with the patient, resident and teaching physician in separate locations) through December 31, 2025. This virtual presence will continue to meet the requirement that the teaching physician be present for the key portion of the service.
Coding Update
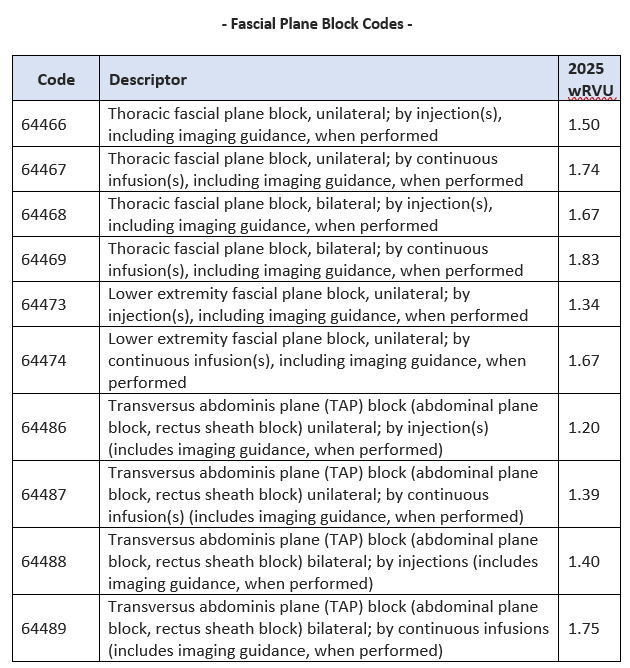
According to the American Society of Anesthesiologists (ASA), CMS finalized the values of several Facial Plane Block codes, which the ASA hails as “a significant win for anesthesiologists and pain medicine physicians.” Starting January 1, 2025, pain medicine physicians—as well as anesthesia providers—will be able to get paid by Medicare for providing thoracic (64466, 64467, 64468, 64469) and lower extremity (64473, 64474) fascial plane block services reported with these new Category I CPT codes. These new thoracic and lower extremity fascial plane block services expand on the existing transversus abdominis plane (TAP) block code family (64486 – 64489). For 2025, CMS finalized the following work RVUs for the fascial plane block codes. The table below reflects CMS’s proposed work RVUs for the fascial plane block codes.
We will be addressing what the 2025 PFS final rule provides relative to the CMS quality programs (such as MIPS) for the upcoming year and how those requirements might affect our readers.
